Difference between Medicaid And Medicare : Facts Explained
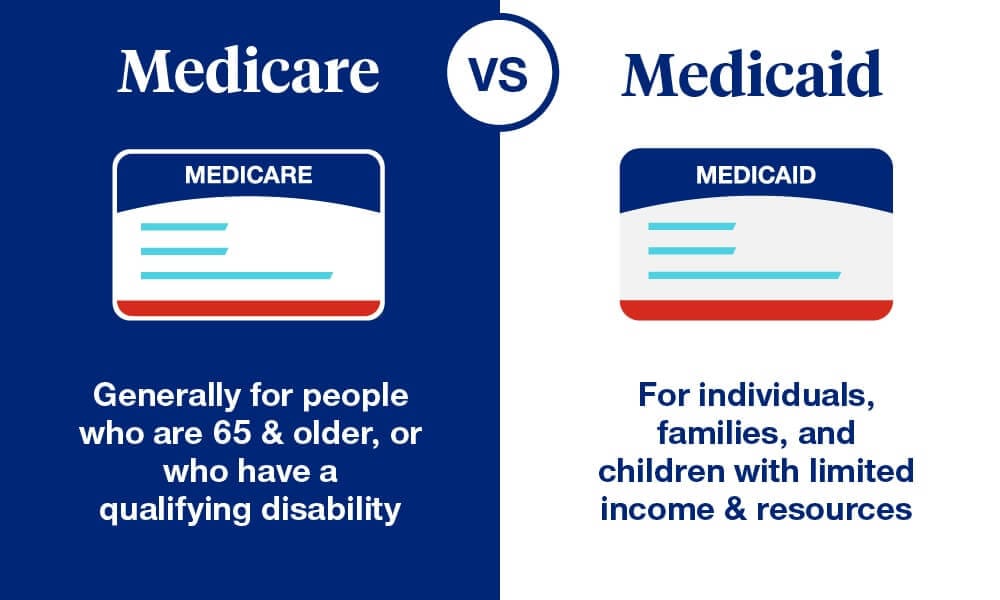
Medicaid is a state and federal program aiding low-income individuals. Medicare is a federal program for those 65 and older or with certain disabilities.
Medicaid and Medicare are crucial components of the American healthcare system, providing essential services to different populations. Medicaid helps low-income individuals and families access healthcare by offering free or low-cost medical benefits. Medicare, on the other hand, serves older adults and individuals with specific disabilities, ensuring they receive necessary medical care.
Both programs aim to reduce healthcare costs and improve health outcomes for their respective groups. Understanding their differences helps individuals and families make informed healthcare decisions. Each program has unique eligibility requirements and benefits, making them vital for various segments of the population.
Key Differences
Medicaid and Medicare serve millions in the United States. Both programs provide health coverage but differ in many ways. Understanding their key differences helps people choose the right program for their needs.
Eligibility Criteria
Medicaid and Medicare have distinct eligibility requirements. Medicaid targets low-income individuals and families. Eligibility depends on income, family size, and state regulations. States may have different guidelines.
Medicare, on the other hand, primarily serves people aged 65 and older. It also covers younger individuals with specific disabilities or conditions. Unlike Medicaid, Medicare eligibility is consistent nationwide.
Here’s a table summarizing the key eligibility criteria:
| Program | Eligibility Criteria |
|---|---|
| Medicaid |
|
| Medicare |
|
Coverage Options
Medicaid offers comprehensive coverage. It includes hospital stays, doctor visits, long-term care, and more. States can offer additional benefits like dental and vision care. Coverage and benefits can vary widely between states.
Medicare is divided into different parts. Each part covers different services:
- Part A: Hospital insurance covering inpatient stays, skilled nursing, and hospice care.
- Part B: Medical insurance for outpatient care, doctor visits, and preventive services.
- Part C: Medicare Advantage Plans, which are private plans offering Parts A and B, and often Part D.
- Part D: Prescription drug coverage.
Medicare coverage is consistent across all states. However, not all services are fully covered. Beneficiaries may need to pay premiums, deductibles, and co-pays.
Credit: www.uhc.com
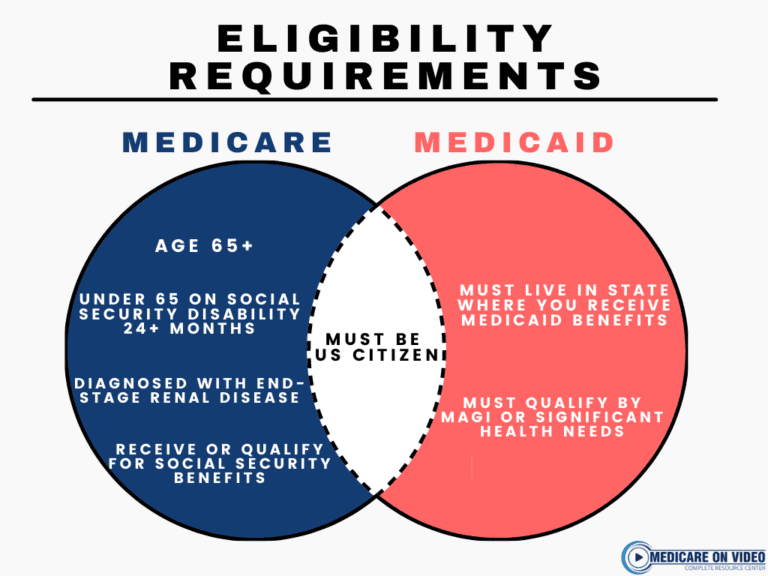
Eligibility Requirements
Medicaid and Medicare are two distinct government programs in the United States that provide healthcare coverage. Understanding the eligibility requirements for each is crucial. These requirements vary significantly, especially regarding age and income. Here’s a closer look at how these factors influence eligibility for Medicaid and Medicare.
Age Criteria
Medicare eligibility is primarily based on age. Individuals 65 years or older qualify for Medicare. This applies regardless of income or employment history. Some younger people with disabilities and those with End-Stage Renal Disease (ESRD) can also qualify.
Medicaid, on the other hand, doesn’t have a strict age requirement. It serves low-income individuals and families of all ages. This includes children, pregnant women, parents, seniors, and people with disabilities. Each state has different rules about eligibility and services.
| Program | Age Requirement |
|---|---|
| Medicare | 65 years or older (some exceptions for disabilities and ESRD) |
| Medicaid | No strict age requirement |
Income Restrictions
Medicaid is designed for individuals with low income. Each state sets its own income limits. These limits are based on the Federal Poverty Level (FPL). For example, a state might cover individuals with an income up to 138% of the FPL.
To qualify for Medicare, income is not a factor. Most people 65 and older are eligible if they or their spouse paid Medicare taxes while working. People under 65 may qualify due to disability. Those who don’t automatically qualify can purchase Medicare by paying premiums.
Here’s a quick comparison of income restrictions:
- Medicaid: Income limits vary by state and are based on the FPL.
- Medicare: No income restrictions for eligibility.
Understanding these differences helps determine which program you or your loved ones may be eligible for. It’s essential to check specific state guidelines for Medicaid as they can vary widely.
Coverage Details
Understanding the differences between Medicaid and Medicare can be confusing. Both are government programs that provide health coverage, but they serve different populations and offer different services. Let’s dive into the coverage details for each program.
Services Covered By Medicare
Medicare is a federal program primarily for people aged 65 and older, but it also covers some younger individuals with disabilities. Medicare has four parts: Part A, Part B, Part C, and Part D.
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Most people do not pay a premium for Part A.
Part B covers certain doctors’ services, outpatient care, medical supplies, and preventive services. There is a monthly premium for Part B.
Part C (Medicare Advantage) is an alternative to Original Medicare. Medicare Advantage plans are offered by private companies approved by Medicare. These plans cover all services under Parts A and B and usually include Part D (prescription drug coverage).
Part D covers prescription drugs. These plans are also offered by private companies and require a monthly premium.
- Inpatient hospital care
- Skilled nursing facility care
- Home health care
- Hospice care
- Doctor visits
- Outpatient care
- Preventive services
- Prescription drugs
Services Covered By Medicaid
Medicaid is a joint federal and state program that provides health coverage to low-income individuals and families. Each state has its own Medicaid program, so coverage can vary. However, there are mandatory benefits that all states must provide.
These mandatory benefits include:
- Inpatient and outpatient hospital services
- Early and periodic screening, diagnostic, and treatment services (EPSDT) for individuals under 21
- Nursing facility services
- Home health services
- Physician services
- Rural health clinic services
- Federally qualified health center services
- Laboratory and X-ray services
- Family planning services
- Freestanding birth center services
- Transportation to medical care
- Tobacco cessation counseling for pregnant women
States can also provide optional benefits such as:
- Prescription drugs
- Case management
- Physical therapy
- Occupational therapy
- Speech, hearing, and language disorder services
- Respiratory care services
- Other diagnostic, screening, preventive, and rehabilitative services
Medicaid offers extensive coverage for those who qualify, ensuring they receive comprehensive medical care.
Credit: medicareonvideo.com
Cost Considerations
Understanding the cost differences between Medicaid and Medicare is crucial for making informed healthcare decisions. Both programs provide vital services, but their costs vary significantly. Here, we explore the cost considerations, focusing on premiums, deductibles, and out-of-pocket expenses.
Premiums And Deductibles
The costs associated with premiums and deductibles differ between Medicaid and Medicare. Medicaid typically has lower costs. In many states, Medicaid enrollees pay no premiums. When they do, these premiums are minimal.
Medicare, on the other hand, involves more substantial costs:
- Part A: Usually free if you or your spouse paid Medicare taxes for at least 10 years.
- Part B: Monthly premiums start at $148.50 in 2021 and may increase based on income.
- Part C (Medicare Advantage): Premiums vary by plan.
- Part D: Prescription drug coverage premiums also vary by plan.
The deductibles also differ:
| Medicaid | Medicare |
|---|---|
| Typically low or zero | Part A: $1,484 per benefit period |
| Varies by state | Part B: $203 annually |
Out-of-pocket Expenses
Out-of-pocket expenses include costs such as co-payments, coinsurance, and other charges not covered by premiums and deductibles. These expenses can add up and vary significantly between Medicaid and Medicare.
Medicaid generally has very low out-of-pocket costs. Many states ensure that beneficiaries have minimal expenses. This includes low or no co-payments for medical services and medications.
Medicare out-of-pocket costs are usually higher. These costs include:
- Part A: Daily coinsurance for hospital stays beyond 60 days.
- Part B: 20% coinsurance for most services after meeting the deductible.
- Part D: Costs vary by plan, including co-payments and coinsurance for medications.
Many people with Medicare buy Medigap policies to help cover these costs. These policies reduce out-of-pocket expenses but come with their own premiums.
Here’s a quick comparison:
| Expense Type | Medicaid | Medicare |
|---|---|---|
| Co-payments | Low or none | Varies by service |
| Coinsurance | Low or none | 20% for Part B |
| Medications | Low or none | Varies by Part D plan |
Application Process
The application process for Medicaid and Medicare is crucial. Understanding these steps ensures a smooth experience. Both programs offer significant benefits, but the application procedures differ.
How To Apply For Medicare
Applying for Medicare is straightforward. Medicare is a federal program mainly for people aged 65 and older. Younger people with disabilities can also qualify.
Here are the steps:
- Check Eligibility: Ensure you meet the age or disability criteria.
- Gather Documents: You need your birth certificate, social security card, and proof of U.S. citizenship or legal residency.
- Apply Online: Visit the Social Security website and fill out the online application form.
- Phone Application: Call Social Security at 1-800-772-1213 to apply over the phone.
- Visit Local Office: You can apply in person at your local Social Security office.
Most people automatically get Medicare Part A (Hospital Insurance) and Medicare Part B (Medical Insurance) when they turn 65. If you don’t receive these benefits automatically, follow the steps above.
The table below summarizes the key points:
| Step | Details |
|---|---|
| Check Eligibility | Age 65 or disability |
| Gather Documents | Birth certificate, social security card |
| Apply Online | Social Security website |
| Phone Application | 1-800-772-1213 |
| Local Office | Visit in person |
How To Apply For Medicaid
Medicaid is a state and federal program for low-income individuals and families. The application process varies by state. Here are the general steps:
- Check Eligibility: Income requirements and other criteria vary by state.
- Gather Documents: You need proof of income, residency, and identification.
- Apply Online: Visit your state’s Medicaid website and complete the application form.
- Phone Application: Call your state’s Medicaid office to apply over the phone.
- Visit Local Office: Apply in person at your local Medicaid office.
Each state has different rules, so ensure you follow your state’s specific guidelines. Many states offer an online portal for easy application. You can also get help from community organizations.
The table below highlights the main steps:
| Step | Details |
|---|---|
| Check Eligibility | State-specific income requirements |
| Gather Documents | Proof of income, residency, ID |
| Apply Online | State Medicaid website |
| Phone Application | State Medicaid office |
| Local Office | Visit in person |
State Variations
The difference between Medicaid and Medicare often confuses people. Understanding state variations is crucial. Both programs offer healthcare coverage, but they operate differently depending on the state. Learning these differences helps you maximize benefits and coverage.
State Medicaid Programs
Medicaid is a joint federal and state program. States have the flexibility to design their own Medicaid programs. This leads to significant variations in coverage and eligibility. Each state sets its own guidelines within federal limits.
Key differences in state Medicaid programs include:
- Eligibility Requirements: Some states cover all low-income adults, while others limit coverage to specific groups like pregnant women and children.
- Benefits: While federal law requires certain benefits, states can offer additional services. For example, some states cover dental and vision care, while others do not.
- Cost-Sharing: States decide on premiums, co-payments, and deductibles. Low-income individuals may have little to no cost-sharing.
Here’s a table illustrating the differences in Medicaid programs in three states:
| State | Eligibility | Additional Benefits | Cost-Sharing |
|---|---|---|---|
| California | Low-income adults, children, pregnant women | Dental, vision, mental health | Minimal co-payments |
| Texas | Low-income children, pregnant women | Limited dental, vision | Higher co-payments |
| New York | Low-income adults, children, pregnant women | Comprehensive dental, vision, mental health | Minimal to no co-payments |
Medicare Adjustments By State
Medicare is a federal program, offering uniform benefits across the country. However, state-specific adjustments can affect your experience. These adjustments often involve Medicare Advantage Plans and Medigap policies.
Key state-specific adjustments in Medicare include:
- Medicare Advantage Plans: These plans are offered by private companies. Availability and specifics vary by state and even by county.
- Medigap Policies: These supplemental plans help cover costs not included in Original Medicare. Some states have additional Medigap protections.
- Prescription Drug Coverage: While Part D is standardized, plan availability and premiums vary by state.
Here’s a table showing variations in Medicare Advantage Plans across three states:
| State | Number of Plans | Average Premium | Additional Benefits |
|---|---|---|---|
| Florida | 50+ | $25/month | Dental, vision, wellness programs |
| Ohio | 40+ | $30/month | Dental, vision, hearing aids |
| Nebraska | 20+ | $35/month | Limited dental, vision |
Dual Eligibility
Medicaid and Medicare are two essential health programs in the U.S. Medicare is designed for people aged 65 or older and those with certain disabilities. Medicaid assists low-income individuals and families. Dual Eligibility means that some people qualify for both Medicaid and Medicare. This can offer comprehensive coverage but comes with its own challenges.
Benefits Of Dual Enrollment
Dual enrollment provides a variety of benefits that can improve healthcare access and affordability. Some of the key advantages include:
- Comprehensive Coverage: You receive benefits from both programs, covering more services.
- Cost Savings: Medicaid can help pay for Medicare premiums, deductibles, and co-payments.
- Prescription Drug Coverage: Medicaid can help with costs not covered by Medicare Part D.
- Extra Support Services: Medicaid offers additional services like long-term care, which Medicare does not.
Let’s look at a simplified comparison:
| Feature | Medicare | Medicaid |
|---|---|---|
| Eligibility | Aged 65+, certain disabilities | Low-income individuals and families |
| Coverage | Hospital, Medical, Prescription Drugs | Broader range, including long-term care |
| Cost | Premiums, Deductibles, Co-payments | Lower costs, additional financial help |
Challenges Faced
Despite the benefits, dual eligibility also comes with challenges. Here are some common issues:
- Complex Coordination: Coordinating between two programs can be confusing.
- Different Rules and Regulations: Each program has its own set of rules, making it hard to navigate.
- Paperwork: Managing the paperwork for both programs is time-consuming.
- Limited Provider Networks: Finding healthcare providers who accept both Medicare and Medicaid can be challenging.
Consider these points:
- Eligibility Criteria: Understanding the different eligibility criteria for each program.
- Approval Processes: Dealing with the separate approval processes for services.
- Billing Issues: Resolving billing issues that arise from dual coverage.
While dual eligibility offers extensive coverage, navigating the complexities requires effort and attention to detail.
Recent Changes
Medicaid and Medicare are both critical programs in the U.S. healthcare system. Recent changes have impacted how each program operates and serves beneficiaries. Understanding these changes is vital for those who rely on these services.
Legislative Updates
In recent years, several legislative updates have significantly altered Medicaid and Medicare.
The Affordable Care Act (ACA) brought major changes to Medicaid. It expanded eligibility, allowing more low-income adults to qualify. States received federal funding to support this expansion.
Medicare also saw changes through the Medicare Access and CHIP Reauthorization Act (MACRA). This law revamped how Medicare pays doctors. It shifted from fee-for-service to value-based care.
- Expansion of Telehealth Services: Both Medicaid and Medicare now cover more telehealth services. This change helps beneficiaries access care from home.
- Drug Pricing Reforms: New rules aim to lower prescription drug costs for Medicare beneficiaries. Medicaid also adopted measures to control drug spending.
- Eligibility Adjustments: Medicaid eligibility criteria have been adjusted in several states. This change affects who can access Medicaid benefits.
| Program | Recent Legislative Changes |
|---|---|
| Medicaid | ACA Expansion, Telehealth, Drug Pricing |
| Medicare | MACRA, Telehealth, Drug Pricing |
Impact On Beneficiaries
These legislative updates have a direct impact on beneficiaries. The expansion of Medicaid under the ACA allowed millions of new individuals to gain coverage. This change reduced the number of uninsured Americans.
Medicare’s shift to value-based care aims to improve patient outcomes. Doctors now focus more on quality than quantity of care. This change benefits Medicare recipients by promoting better health management.
Telehealth services have become more accessible. Beneficiaries in both programs can now have virtual doctor visits. This change is especially helpful for those in rural areas or with mobility issues.
- Lower Prescription Costs: New drug pricing reforms mean lower out-of-pocket costs for medications. This change is beneficial for those on fixed incomes.
- Improved Care Access: More people now qualify for Medicaid. This change helps low-income families access necessary healthcare services.
- Quality Over Quantity: Medicare’s value-based care model encourages better treatment outcomes. Beneficiaries receive more personalized and effective care.
Overall, these changes aim to improve healthcare access and affordability for millions of Americans.

Credit: www.researchgate.net
Frequently Asked Questions
What Is Medicaid?
Medicaid is a state and federal program. It provides healthcare to low-income individuals and families. Eligibility varies by state.
What Is Medicare?
Medicare is a federal program. It provides healthcare to people aged 65 and older. It also serves younger individuals with disabilities.
Who Qualifies For Medicaid?
Eligibility for Medicaid depends on income and family size. It varies by state. Generally, it serves low-income individuals and families.
Who Qualifies For Medicare?
Medicare is available to those aged 65 and older. It also serves younger individuals with certain disabilities or end-stage renal disease.
Conclusion
Understanding the differences between Medicaid and Medicare helps you make informed healthcare decisions. Medicaid supports low-income individuals, while Medicare serves those over 65 or with disabilities. Knowing eligibility and benefits ensures you maximize these programs effectively. Stay informed to navigate healthcare options confidently and secure the best care for your needs.
Read More: